What is PTLD?
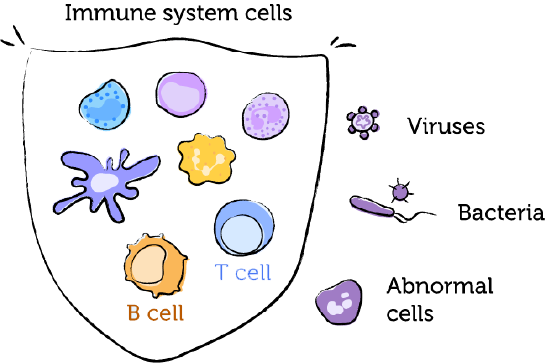
‘Lympho’ refers to lymphocytes, a type of white blood cell.
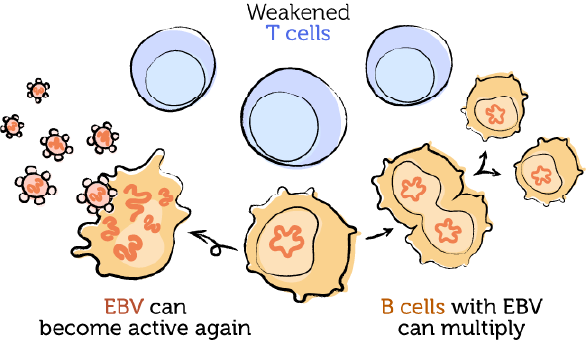
‘Proliferative’ means growing or multiplying quickly.

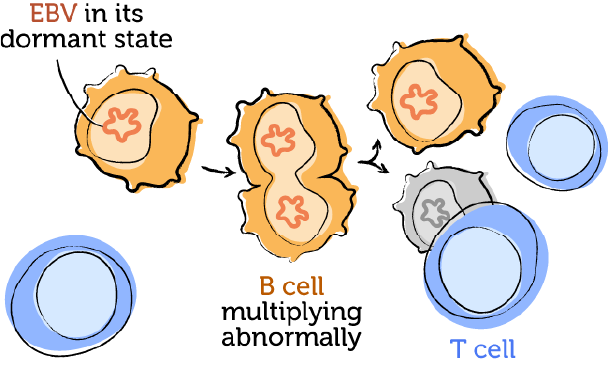
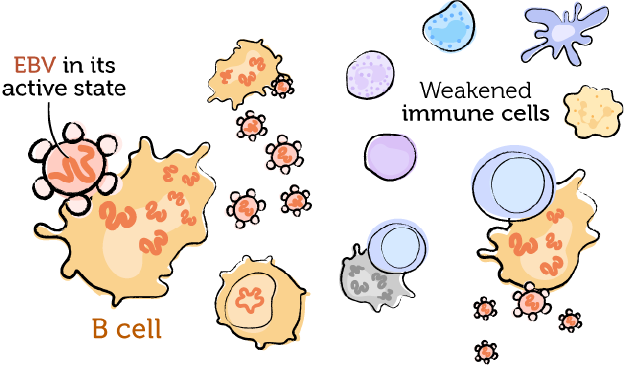
PTLD is when your lymphocytes grow out of control after a transplant. It can develop in anyone taking immunosuppressants after a transplant.
PTLD is a group of diseases. It includes certain kinds of growths and lymphomas. PTLD can become life-threatening. It needs to be brought up to the transplant team so they can diagnose and treat it quickly.
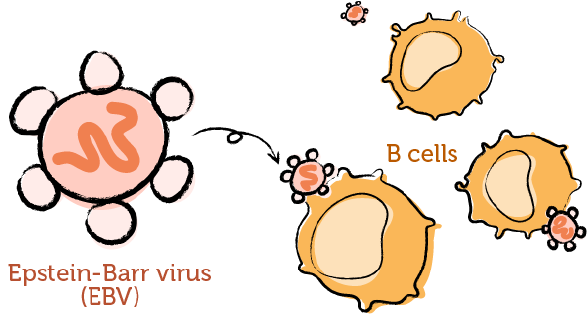
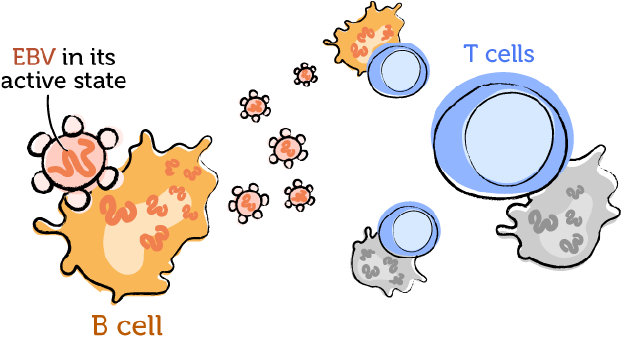
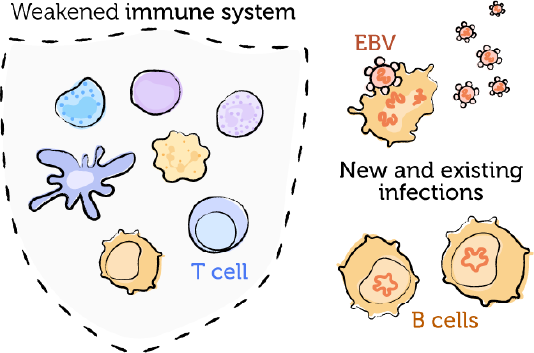
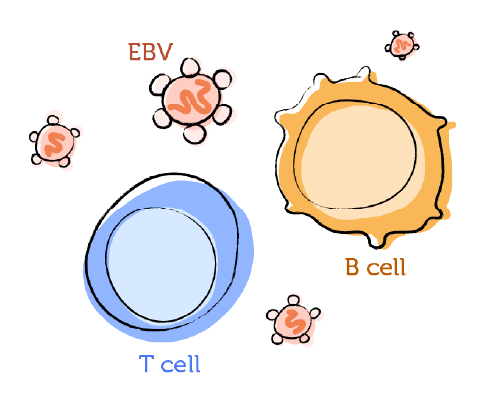
PTLD is often linked to the Epstein‑Barr virus (EBV) . If there is a link, it's called EBV‑positive PTLD. If there is no link, it's called EBV‑negative PTLD.
Anyone taking immunosuppressants after a transplant is at risk for PTLD:
After a blood stem cell transplant, immunosuppressants are needed to prevent graft-versus-host disease (GvHD). However, these medications come with the risk of developing PTLD.
PTLD tends to develop within one year of the transplant. Nearly all cases of PTLD are linked to EBV.
You may have a higher risk of developing PTLD if you:
- received a donor graft that has gone through T-cell removal
- had an unrelated or mismatched stem cell donor
- have never had an EBV infection before the transplant (more common in patients under 10 years old)
- are over 60 years old with a weaker immune system
- have certain genes that affect the immune system

- How long do I have to take immunosuppressants for?
- What is my risk for developing PTLD?
- If I am at risk for PTLD, why do I need to keep taking my immunosuppressants?
- How will I be monitored for PTLD?
Your transplant team monitors the health of your transplant. They also look for signs of post‑transplant complications, including PTLD.
The symptoms of PTLD are broad. They can overlap with symptoms of other conditions. Symptoms can be different in different people, and may include:
- a general change in how you are feeling
- swollen lymph nodes
- unexplained weight loss over a few weeks
- fever or night sweats
- sore throat
- fatigue
- chronic sinus congestion
- severe abdominal pain
- no appetite, nausea, or vomiting
- black or bloody stools

These symptoms may not mean you have PTLD, but they should be looked at by your transplant team
If you notice anything new or a general change in how you're feeling, tell your transplant team or healthcare provider right away. Don't wait until your next appointment.
If you see a healthcare provider other than your transplant team, including in urgent care or the emergency room, tell them about your transplant and immunosuppressants. They may need to reach your transplant team.
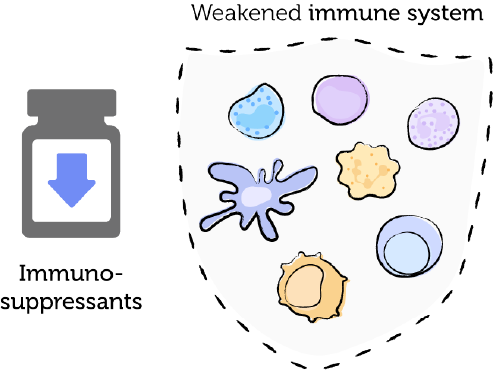
After a transplant, the immune system needs to be weakened with immunosuppressants. This is an important part of preventing rejection or graft-versus-host disease (GvHD) and keeping the transplant healthy. When the immune system is weak, an EBV infection can become active. This can increase the risk of EBV‑positive PTLD. Scientists are still studying what causes EBV‑negative PTLD.
Read more below to see the details.