Diagnosis
and treatment
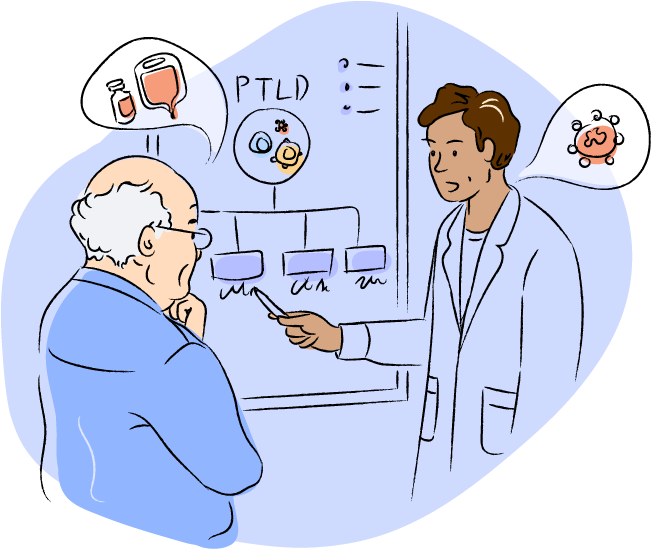
PTLD is related to your transplant and immunosuppressants. Your transplant team needs to be aware so they can diagnose and treat it quickly.

 How is PTLD diagnosed?
How is PTLD diagnosed?
Your transplant team will review your medical and transplant history. They may also ask you to meet with other healthcare providers. You may have to go in for:
- blood
- bone marrow
- cerebral spinal fluid (if the doctor suspects the central nervous system is involved)
- CT scan
- PET scan
- MRI
Afterwards, your transplant team will run tests on the tissue samples and analyze the results.
Two important tests are
immunophenotyping and looking at levels of EBV.
Ask your transplant team if you have questions about PTLD. You can do this even if you haven’t seen them in a while. They are the experts on your transplant history and the immunosuppressants you are taking.
If you can’t see your transplant team right away, see your primary care provider, or if under 18, a pediatrician. They may be able to reach the transplant team for you.

- What are the tests that I need to have done?
- What can I do to prepare for these tests?
- How long do these tests take and when will the results come back?
PTLDs range from mild, benign growths to aggressive cancers.
When your transplant team is analyzing the results of diagnostic tests, they are trying to understand:- the type of lymphocyte that is affected
- if EBV is involved
- the type of growth or lymphoma it is
PTLD affects your lymphocytes. In most cases, your B cells are affected, but PTLD can also affect T cells and natural killer (NK) cells.
EBV can be linked to the development of PTLD. If there is a link to EBV, it's called EBV‑positive PTLD. If there is no link, it's called EBV‑negative PTLD.
The World Health Organization (WHO) has four categories for growths and lymphomas that are considered PTLDs. You may hear your doctor use these categories or the name of the growth or lymphoma.

- your general health and medical history
- the type of PTLD you have
- what treatments you've had
- whether your PTLD is new or has come back
Immunotherapies work by helping the immune system to fight a disease.
Your immunosuppressants may be carefully adjusted by your transplant team. This is done to help your immune system control PTLD while keeping your transplant healthy.
EBV-directed therapy targets and kills cells that are infected by EBV. It is used to treat diseases linked to EBV, including EBV‑positive PTLD.
Antibody therapy helps the immune system recognize and fight specific cells. In PTLD, it may be used to target B cells.
Surgery and radiotherapy are not usually used to treat PTLD. They may be used to control or reduce symptoms.

CAR T-cell therapy is made from the patient’s T cells. The patient’s T cells are genetically modified in the lab to attack specific types of cancer cells.
Clinical trials are research studies. In a clinical trial, patients may receive an existing treatment or a new treatment that is being studied.

Chemotherapy kills cells that grow and multiply quickly, including cancer cells. When it is used with antibody therapy, it’s called chemo-immunotherapy.

There may be other treatment options not listed here.

Your transplant team will need to be involved. This is because PTLD is related to your transplant and immunosuppressants. You may also see other specialists, depending on your transplant type, age, and other health conditions.
If you had a solid organ transplant, you may see:
- your transplant team
- a blood cancer specialist (also called a hematologist‑oncologist or heme‑onc)
- other specialists, such as pediatricians, organ specialists, and radiologists
If you had a blood stem cell transplant, you may see:
- your heme-onc who performed the transplant
- other specialists, such as pediatricians and radiologists

- Who might be involved in my PTLD diagnosis and treatment?
- How often will I see the different people involved?
- Who will be my main point of contact?